- Select 6 measures to report
- 1 outcome or high-priority measure
- Select from individual measures or a specialty measure set

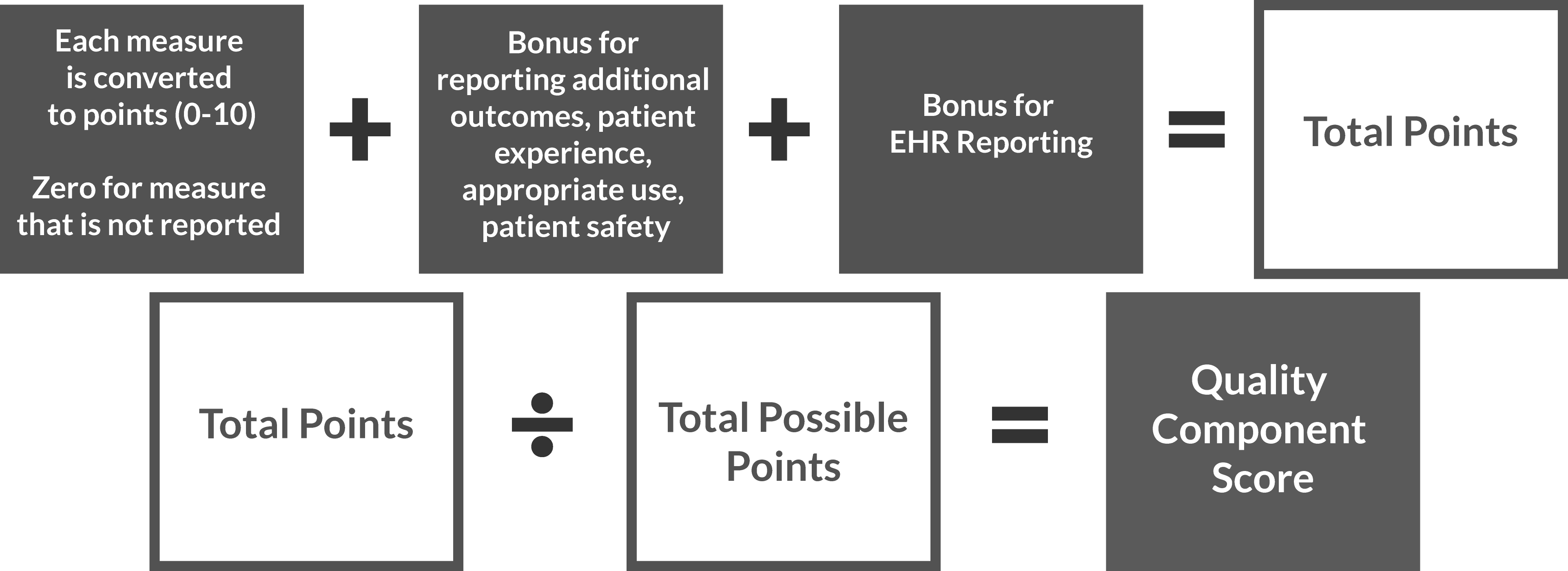
The Quality Performance category is closely related to the Physician Quality Reporting System (PQRS). The 2016 PQRS requirements have been relaxed [now requiring 6 measures to be reported as opposed to 9] and the measures list has been updated with additional measures available.
CMS has removed the previously available Measures Group option where physicians could report on 20 patients via a registry. Providers must report on 75% of all patients, if reporting via registry or EHR.
For PQRS, eligible groups or clinicians had to report 50% of all eligible instances (using only Medicare Part B patient encounters) for individual measure reporting, or 20 unique patients for measure group reporting. For MIPS, measure groups are no longer an option, and 75% of patients from all payers must be reported on.
For PQRS, eligible groups or clinicians using individual measures had to report 9 measures covering 3 National Quality Strategy (NQS) domains, including one cross-cutting measure. For MIPS, the requirement is only 6 measures. As a part of those 6 measures, one of those measures must be an outcome based measure. If there is no applicable outcome measure, than a high priority measure may be used instead. There is also no NQS domain requirement under MIPS.
For PQRS in 2016, reporting successfully only achieved penalty avoidance. For MIPS, the ability to gain an incentive returns and is greater than it ever was under PQRS. Highly performing groups or clinicians can earn up to a 9% incentive for having an exceptional MIPS Composite Score for program year 2026.
- Submission
- Scoring
An organization may choose to submit measure data to CMS as an individual or as a group through any the options below.
| Method | Individual Submisson | Group Submission |
|---|---|---|
| Qualified Registry |  |
 |
| EHR |  |
 |
| Claims |  |
 |
Talk to our Quality Payment Program specialists to learn how we can help.