- Solutions
Solutions
- Pricing
- Company
Company
- Resources
Resources
- Request Demo
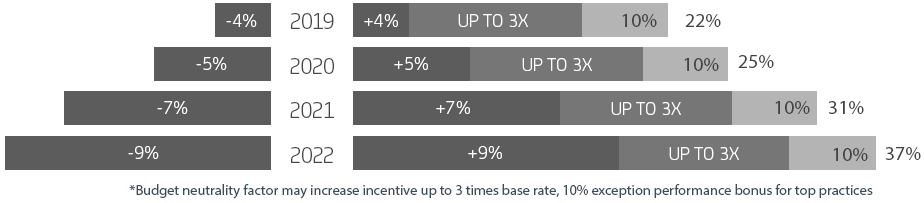
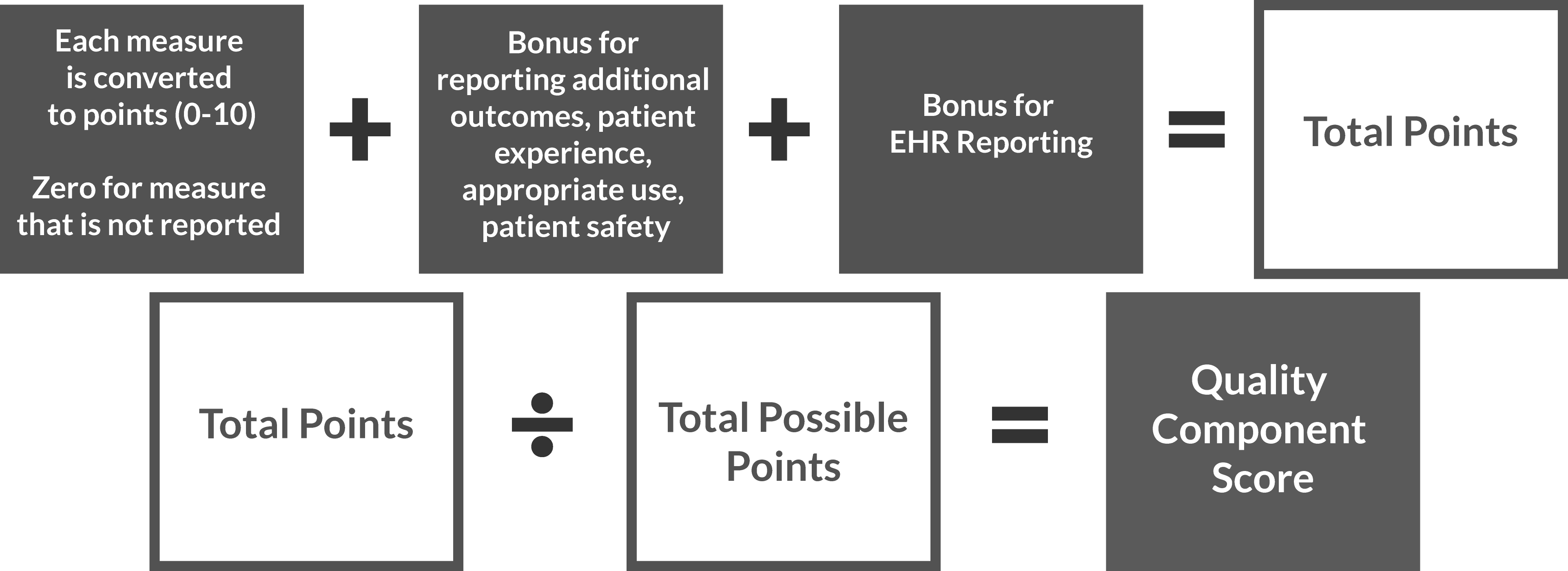
Much like the Value Based Modifier (VBM) program that ends in 2017, Merit-Based Incentive Payment System (MIPS) will determine eligible clinicians’ payment adjustments based on how they rank versus their peers in the measures defined by CMS. The score that will be used to determine the performance threshold for MIPS is called the MIPS Composite Performance Score.
Minimum and maximum adjustment for full MIPS participation.
Talk to our Quality Payment Program specialists to learn how we can help. Visit MIPS Consulting Services for more information.

Tell us about yourself & a CureMD Consultant will contact you shortly.